Pediatric Blood Draw Limits
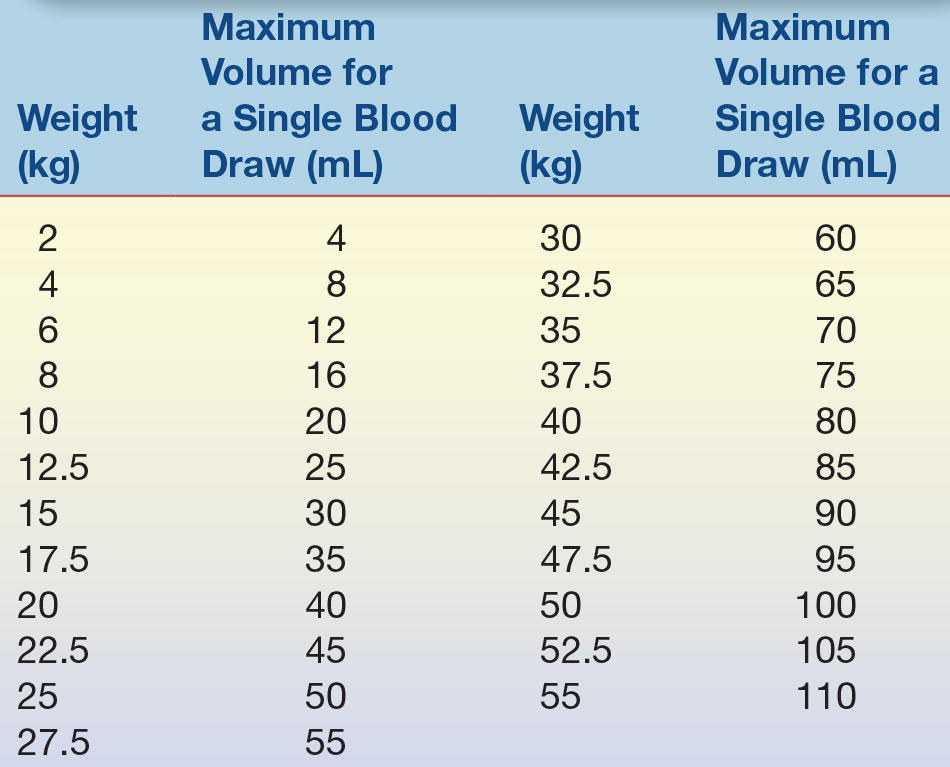
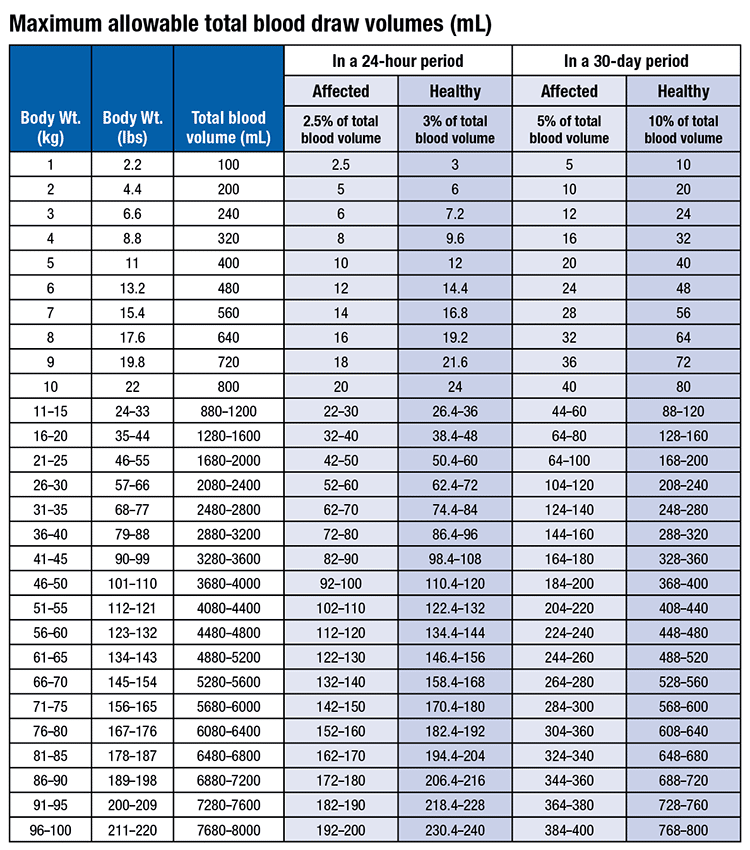
Pediatric Blood Draw Limits - The chapter includes background information ( section 2.1 ), practical guidance ( section 2.2 ) and illustrations ( section 2.3 ) relevant to best practices in phlebotomy. The number was lower than what the research team expected. Camille santos, quenby mahood cite as: Existing guidelines specify paediatric blood. Web chla irb blood draw volume policy. One blood draw ( = 2.5% of total blood volume) 1 2.2 100 2.5 2 4.4 200 5 3 6.3 240 6 4 8.8 320 8 5 11 400 10 6 13.2 480 12. 3% total blood/24 hour period 10% total blood/month For outpatient phlebotomy, observe the patient for the risk of development of physiologic signs of rapid blood loss. Isbn 978 92 4 159922 1 (nlm classification: The total blood volume can be. Isbn 978 92 4 159922 1 (nlm classification: The total blood volume can be. Symptoms of excessive blood loss are tachycardia, decreased profusion, bradycardia, decrease in blood pressure, and shock. 75 ml/kg for children over the age of 3 months; However, the gold standard is. The below blood volume limits. Web in order to reduce the risks associated with phlebotomy draws on pediatric patients the following guidelines have been established: Web this chapter discusses aspects specific to paediatric and neonatal blood sampling ( 60, 61 ). Web this chapter covers all the steps recommended for safe phlebotomy and reiterates the accepted principles for blood drawing. Camille santos, quenby mahood cite as: Web max drawn in one blood draw: Maximum drawn in a 30 day period : 100 ml/kg for premature infants; Web this chapter covers all the steps recommended for safe phlebotomy and reiterates the accepted principles for blood drawing and blood collection. Piazza noted that introductions and building a rapport lessen a child’s anxiety. Web in addition to the universal screening recommended at 12 months of age to detect iron deficiency anemia, physicians should conduct a risk assessment to determine if hematocrit or hemoglobin. The number was lower than what the research team expected. (example 5kg baby would have 500ml total blood. 2.5% of total blood volume: Web allowable blood draw limits for pediatric research: 70 ml/kg for male adolescents; Email from department of pediatrics 10/27/2007. Pounds are listed in the second column. For outpatient phlebotomy, observe the patient for the risk of development of physiologic signs of rapid blood loss. Web in order to reduce the risks associated with phlebotomy draws on pediatric patients the following guidelines have been established: Maximum drawn in a 30 day period : Piazza noted that introductions and building a rapport lessen a child’s anxiety. Camille santos,. Web this chapter discusses aspects specific to paediatric and neonatal blood sampling ( 60, 61 ). 5% of total blood volume: Web the age factor equals: Healthy and having no or minimal blood draws for clinical purposes the total blood volume withdrawal allowance would be: Web five studies and nine guidelines were identified. Web safe draw limits: The below blood volume limits. Email from department of pediatrics 8/28/2010. Wb 381) © world health organization 2010 Symptoms are more severe with acute loss. 100 ml/kg for premature infants; Web recommendations for maximum blood draw in children range from 1 to 5% despite limited evidence. Web in order to reduce the risks associated with phlebotomy draws on pediatric patients the following guidelines have been established: Web cadth reference list maximum blood draw for pediatric patients march 2022 summary of abstracts authors: Symptoms of excessive. Anyone taking blood from children and neonates must be well trained and practiced in venepuncture techniques. Web pediatric blood volume draw guidance the table below provides guidance for clinical researchers and reb reviewers for assessing the risk level associated with total blood volumes collected in pediatric research participants for. Pounds are listed in the second column. Healthy and having no. Existing guidelines specify paediatric blood. Web five studies and nine guidelines were identified. Anyone taking blood from children and neonates must be well trained and practiced in venepuncture techniques. Web this chapter covers all the steps recommended for safe phlebotomy and reiterates the accepted principles for blood drawing and blood collection. Isbn 978 92 4 159922 1 (nlm classification: 100 ml/kg for premature infants; No more than 2.5% of total blood volume may be drawn solely for research purposes within a 24 hour period. Web recommendations for maximum blood draw in children range from 1 to 5% despite limited evidence. Web in addition to the universal screening recommended at 12 months of age to detect iron deficiency anemia, physicians should conduct a risk assessment to determine if hematocrit or hemoglobin. Email from department of pediatrics 10/27/2007. Web this chapter discusses aspects specific to paediatric and neonatal blood sampling ( 60, 61 ). 5% of total blood volume: Piazza noted that introductions and building a rapport lessen a child’s anxiety. The following chart states the maximum blood volume for pediatric draws based on. Pounds are listed in the second column. Web chla irb blood draw volume policy.
How To Draw Blood With Ease From Children

maximum allowable total blood draw volumes (clinical + research)

How To Draw Pediatric Blood Bornmodernbaby
How To Draw Pediatric Blood Bornmodernbaby

Pediatric Vital Signs Reference Chart Pediatric vital signs

Blood Culture Indications, Timing, and Volume • Microbe Online

Pediatric Blood Draw Guidelines Warehouse of Ideas
How To Draw Pediatric Blood Bornmodernbaby
I am updating our procedure for blood draw volume limits and using So

Pediatric Blood Draws Pediatric Nursing Lecturio Nursing YouTube
3% Total Blood/24 Hour Period 10% Total Blood/Month
Email From Department Of Pediatrics 8/28/2010.
Typically, A Blood Draw Is Quick And Easy;
The Chapter Includes Background Information ( Section 2.1 ), Practical Guidance ( Section 2.2 ) And Illustrations ( Section 2.3 ) Relevant To Best Practices In Phlebotomy.
Related Post: